Part 4: The immunisation programme
4.1
In this Part, we describe how the immunisation programme is structured, the broad approach to strategy and planning, and the approach to risk management. We also describe the governance and advisory groups that support the immunisation programme, the planning that has been completed to date, and what still needed to be done at the time our audit was completed.
4.2
For the immunisation programme to be successful, we expected to see a dedicated programme team that is adequately resourced and supported by the leadership of the Ministry. We expected the immunisation programme to be designed to work at pace and be well supported by appropriate governance arrangements, including access to both technical advice and broader input from stakeholders with expertise in public health and immunisation.
4.3
We expected to see an immunisation strategy in place to provide direction to the immunisation programme and guide planning. By this stage in the programme, we expected to see a reasonably detailed operational plan to implement the immunisation strategy, with the main elements and critical path clearly identified and regular monitoring and reporting to governance against critical milestones and key risks.
4.4
We expected both the immunisation programme’s structure and plans to reflect how the Ministry would achieve its stated objectives to uphold the principles of te Tiriti o Waitangi11 and provide equitable access to the vaccine for Māori and Pasifika communities, people with disabilities, and harder-to-reach communities.
Summary of findings
4.5
A dedicated immunisation programme team has been established, and the programme has been designed to operate at pace. The programme structure – made of separate “design and build” and “run” components – allowed for vaccinations to begin in limited settings from February 2021 with the roll-out of vaccinations to groups three and four being planned at the same time.
4.6
This approach enabled the Ministry to make progress and learn from early experience. However, it has also created some problems. The urgency to start vaccinating meant that, early on, key resources were not sufficiently focused on designing the nationwide roll-out, which contributed to delays in planning. Aspects of the early programme structure, such as having multiple Senior Responsible Officers, confused accountabilities and slowed decision-making.
4.7
The Ministry identified these issues and restructured the immunisation programme. Recent changes reduced the number of Senior Responsible Officers to one. Although these changes have been necessary and demonstrated the immunisation programme’s ability to adapt, it is likely they have also slowed progress.
4.8
Some of the processes and systems that have supported the early roll-out of vaccinations will need to change when vaccinations are rolled out at a larger scale. At the time of our audit, the plan to scale up had not been fully worked through. The Ministry was not able to provide us with clear and consistent information about its overall plan. In our view, more time spent on developing the strategy could have provided better direction for decision-making and supported more efficient planning.
4.9
An experienced governance group provides advice to the immunisation programme, and there are arrangements in place to provide additional real-time assurance and advice. Several advisory groups are also in place to provide technical and clinical advice to the programme team and advice on how to ensure equitable delivery of the vaccine. Members of these groups bring significant expertise and a range of views to inform decision-making about programme design and implementation. The immunisation programme also has specific arrangements designed to monitor and provide ongoing advice about the safety of the vaccines.
4.10
Ensuring te Tiriti obligations and equity objectives are met is a key focus for the immunisation programme. Although accountability for this work was not initially clear, changes have been made to rectify this and ensure that it is properly resourced. Ongoing focus is needed on this aspect of the programme to ensure that it translates into tangible outcomes for Māori and Pasifika communities, people with disabilities, and harder-to-reach communities.
The immunisation programme’s approach and structure
4.11
Figure 1 shows the three broad phases of activity that underpin the immunisation programme’s approach: “Covid-19 design and build”, “Covid-19 run”, and “Business as usual (BAU) immunisation”. These phases are not in a strictly linear sequence, and there is some overlap between them.
Figure 1
The three phases of the immunisation programme
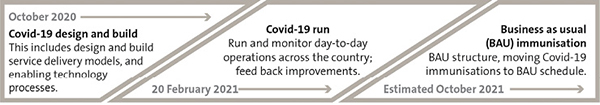
Source: Adapted from planning documents supplied by the Ministry of Health.
4.12
This approach allowed vaccinations to start early in limited settings while planning for the roll-out to other groups progressed. It also meant that lessons from early “Covid-19 run” activities could be fed back into the “Covid-19 design and build” phase to improve implementation of later “Covid-19 run” activities.
4.13
The Ministry’s programme team is also using a planning approach that enables the immunisation programme to move at pace and allow it to be responsive to changes in the environment. The immunisation programme is organised into a series of smaller activities, called sprints. Each sprint takes two weeks and involves teams working on a series of short-term goals. The focus of each sprint is currently planned out to the start of July 2021, which is when the roll-out moves to the general population. This is when all elements of the immunisation programme need to be ready.
The programme structure has changed a number of times
4.14
When we started our audit, the immunisation programme had a complicated structure that reflected, in part, the programme’s complexity. The programme had four Senior Responsible Officers12 who were each responsible for different parts of the programme. This was reduced to two in mid-March 2021 and then to one in early April 2021.
4.15
In February 2021, there were concerns both internally and externally that equitable access to the vaccine was not being properly incorporated into the immunisation programme. Although there were te Tiriti and equity leads in place from November 2020, and information was being developed to help inform district health board programme design, there were concerns that accountabilities were not clear.
4.16
It was also not clear how equity considerations would be factored into the way the vaccine was rolled out. At that time, strategies to support equity were still to be produced.
4.17
In early March 2021, the equity team was expanded to include dedicated leads for Māori, Pasifika, and disability considerations, along with additional support staff. Staff were drawn from the Māori Health Directorate and Pacific Health Team within the Ministry. There was also a Māori communications team established within the wider vaccine communications team. Māori and Pasifika strategies were prepared and finalised by 8 March 2021.
4.18
Changes to the programme’s structure in April 2021 saw the te Tiriti and equity responsibilities combined under the new role of General Manager Equity. That role is now responsible for leading and co-ordinating all equity work and ensuring that it is embedded in decisions about the design of the immunisation programme.
4.19
The separation between the “Covid-19 design and build” and “Covid-19 run” parts of the programme (see Figure 1) created some problems. A significant number of staff had more than one main focus. Early on, as the “Covid-19 run” phase progressed, several staff supporting the “Covid-19 design and build” phase were diverted. This delayed important parts of the programme’s design. Members of the programme team we spoke to told us about a lack of integration across the immunisation programme, which also created confusion.
4.20
It is understandable that as these issues were identified, the immunisation programme’s structure needed to be adapted. The Ministry has taken steps at various points to simplify the programme’s structure and to clarify and strengthen lines of accountability. In early April 2021, further changes were made to the programme’s structure to bring the “Covid-19 design and build” and “Covid-19 run” phases of the programme together and further reduce the number of Senior Responsible Officers.
4.21
The immunisation programme is now made up of eight workstreams, all of which report to the single Senior Responsible Officer, the National Director Covid-19 Vaccination Implementation Programme. The Senior Responsible Officer reports directly to the Director-General of Health, who reports to a group of Ministers (collectively referred to as the Vaccine Ministers).13
4.22
The eight workstreams cover both the design and run elements of the immunisation programme. Two additional elements – implementation and support – have been added to the structure. The Senior Responsible Officer, the eight workstream leads, and others with a strategy or programme support role comprise the Programme Leadership Group, which meets twice daily to oversee the immunisation programme. Figure 2 provides a summary of the programme’s structure.
Figure 2
Programme structure, as at April 2021
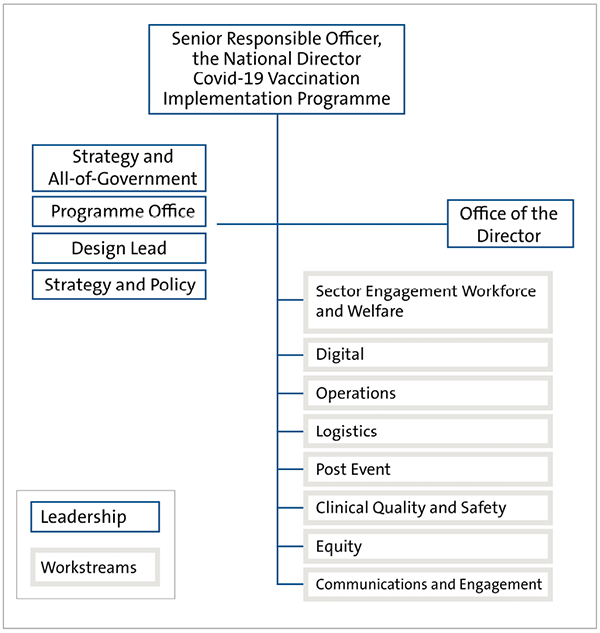
Source: Adapted from planning documents supplied by the Ministry of Health.
4.23
There are also several governance arrangements in place that support the immunisation programme (see paragraph 4.28).
4.24
In our view, clear roles and responsibilities are necessary for accountability. The changes described above show the immunisation programme can adapt as required. However, frequent changes in a short period can also create confusion and might have contributed to delays. In our view, the Ministry should try to limit further changes, especially to lines of accountability.
Resourcing the programme team is an ongoing challenge
4.25
The immunisation programme has drawn on a large number of Ministry staff. Additional resources and expertise have been brought in where required. People from the public and private sectors (including from district health boards) have been seconded into key positions.
4.26
Despite this, many people involved with the immunisation programme have been working long hours for many weeks. Some people have moved onto the immunisation programme after working on the Ministry’s Covid-19 response activities.
4.27
The sustainability of workloads for key staff has been consistently identified as a risk. Specific actions have been taken to mitigate this risk such as developing resource plans and ongoing recruitment of staff. As of mid-April 2021, all programme leadership positions were filled. We were told that none of these people had key responsibilities that would divert them from the immunisation programme in the event of a Covid-19 community outbreak.
Governance and oversight
4.28
The Programme Leadership Group reports to a Steering Group, which is chaired by the Director-General of Health. The Group is comprised of Ministry of Health senior managers and the chief executives of two district health boards.
4.29
The Governance Group provides oversight and assurance. The Governance Group does not make decisions. Its role is to provide advice, both to the Ministry and directly to Ministers. Figure 3 shows the governance structure.
Figure 3
Governance structure, as at April 2021
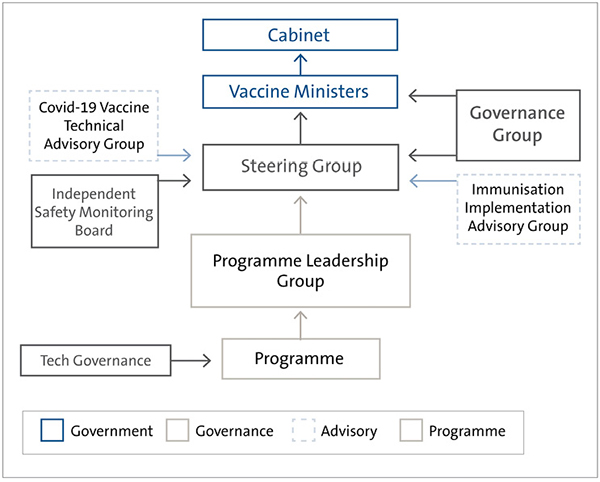
Source: Adapted from planning documents supplied by the Ministry of Health.
4.30
Two members of the Governance Group are from the Ministry: the Director-General of Health and the Deputy Director-General, Māori Health. The group is chaired by a senior experienced health and disability sector leader. Other members include the chief executives of MFAT and the Ministry for Business, Innovation and Employment, a previous government Minister, a private sector leader in information technology, a leader from the Māori community, and a health leader from the Pasifika community.
4.31
The Deputy Director-General, Māori Health is part of both the Governance Group and Steering Group. This role is designed to ensure that te Tiriti responsibilities are being considered throughout the immunisation programme.
There are a range of advisory arrangements in place
4.32
The immunisation programme also relies on several external advisory groups to provide advice on clinical matters, implementation, and safety. The main groups are the Immunisation Implementation Advisory Group, the Technical Advisory Group, and the Independent Safety Monitoring Board. Through these groups, the Ministry has access to people with extensive clinical, scientific, and immunisation expertise.
4.33
The Immunisation Implementation Advisory Group provides advice on vaccine implementation. This Group has played a key role in advising the Ministry on how to ensure that the immunisation programme is designed and implemented in a way that ensures that there is equity, particularly for Māori, Pasifika, people in aged care, and people with disabilities. Initially, the Group did not include a disabilities or aged care perspective. This was seen as a significant gap and a disabilities representative was included in January 2021, and an aged-care representative was included in February 2021.
4.34
The Technical Advisory Group provides technical advice about vaccine use to the immunisation programme. The main role of the Group is to provide clinical advice, such as how long people need to be monitored after they have received the vaccine.
4.35
More specific safety advice is provided by the Independent Safety Monitoring Board. Although the Pfizer vaccine has been provisionally approved for use by Medsafe, monitoring still needs to be carried out as the vaccine is administered more widely. The role of the Independent Safety Monitoring Board is to provide independent assurance about the safety of the vaccine during the roll-out.
4.36
The Independent Safety Monitoring Board provides a level of safety assurance over and above what is standard for immunisation programmes. There was consensus across those we interviewed that, collectively, the Technical Advisory Group and the Independent Safety Monitoring Board provide sufficient clinical and safety advice to the immunisation programme. Processes and systems are in place to ensure that the safety of the vaccine is monitored and managed.
Programme governance is supported with good information
4.37
Considerable resources have been applied to reporting to those governing and steering the immunisation programme. This includes daily reports to Ministers, and regular verbal and written reporting to both the Governance and Steering Groups as part of their respective fortnightly and weekly meeting cycles.
4.38
The reporting to the Governance and Steering Groups includes a number of standing items, including reporting on risks. Our observations of the detailed minutes from those meetings, and from people we spoke with, is that there are free, frank, and robust discussions taking place.
Strategy and planning
4.39
In August 2020, Cabinet invited the Ministry to report back on developing an immunisation strategy for Covid-19. The Ministry has not been able to provide us with a copy of an immunisation strategy. However, a Cabinet paper submitted by the Minister of Health, Associate Minister of Health, and the Minister for Covid-19 Response in December 2020 indicated that the purpose of the immunisation strategy would be to support “best use” of the vaccine, while upholding te Tiriti obligations and promoting equity.
4.40
The Cabinet paper set out four principles to guide the immunisation approach. These were that:
- Covid-19 vaccines would be free and safe;
- the roll-out would be sequenced as the Covid-19 vaccines became available;
- the sequencing of access would be based on need; and
- border settings and the roll-out strategy would continue until there was confidence that the New Zealand population is sufficiently protected.
4.41
The Ministry did not develop the strategy further. Instead it focused on planning for the vaccine roll-out. We understand that Ministers and the Ministry were trying to move the immunisation programme forward as quickly as possible.
4.42
n line with the immunisation programme’s approach, vaccinations have started to be rolled out in limited settings before the detailed design for the roll-out to all groups is complete. As discussed in paragraph 4.12, this has some clear benefits. The Ministry and district health boards have been able to test some key processes and show early progress.
4.43
However, some processes and systems that have supported vaccinations to date will not be the same when vaccinations are rolled out on a larger scale. It has been difficult for the Ministry to provide us with a clear and consistent picture of what has been done and what is left to do to scale up to support the roll-out to all groups. At the time we completed our audit, the critical path had only recently been identified.
4.44
In our view, more time could have been spent formulating a high-level strategy before detailed planning began. We consider that a well thought-out strategy could have provided direction for decision-making and supported more efficient planning. It is unclear to us how much consideration was given to identifying and weighing up the main trade-offs, for example:
- Simplicity and equity – should the immunisation programme prioritise volume of vaccinations over providing access to harder-to-reach communities?
- Use of existing capacity or building new capacity – should the immunisation programme focus on pushing vaccinations through existing channels or create new ones?
- Speed or certainty – how much time will it take to ensure that there is key infrastructure in place, and do the risks of moving quickly outweigh the risks of delay if things do not go as planned?
4.45
Although the key issues are being thought through as the immunisation programme progresses, we saw evidence that some decisions were re-litigated late. Other decisions are being made later than is desirable. This has placed additional pressure on the programme. Some of this might have been avoided if there was a clearer strategic framework to guide design decisions. In our view, the principles identified in the Cabinet paper in December 2020 are helpful but not sufficient to provide this guidance.
4.46
We also consider that some work could have started earlier. We have heard that the uncertainty about which vaccine would be used hampered early planning. In our view, there are many important aspects of the roll-out that could have been planned for without needing to know which vaccine will be used. For example, building a workforce of vaccinators. Similarly, the way in which the wider health and disability sector would be used to support the roll-out could have been determined and communicated earlier.
Much operational planning is being done by district health boards
4.47
When we started this audit, we heard a lot of confusion about exactly how roles and responsibilities were split between the Ministry and district health boards. This was despite a few district health boards having already started vaccinating border workers. The Ministry was not in a position to clarify roles and responsibilities because its detailed planning was not far enough advanced.
4.48
We have since clarified that the Ministry is responsible for the design of delivery models and training pathways for vaccinators and support staff. It will also be responsible for distributing the vaccine to district health boards. Because of the storage requirements of the Pfizer vaccine, distribution will have short lead times. District health boards have to give the Ministry 48 hours’ notice of how many doses of the vaccine they need and where it needs to go. The Ministry told us that during late March and April 2021 it was working with logistics teams in district health boards to further develop processes and systems to be more flexible and responsive to need.
4.49
District health boards and, where applicable, primary health care providers will be responsible for:
- arranging and setting up vaccination sites;
- finding suitably qualified staff to run the vaccination sites and to prepare and administer the vaccines; and
- purchasing some of the equipment that will be needed, except for consumables provided by the Ministry (see paragraph 5.51).
4.50
District health boards will be required to follow guidelines set by the Ministry, meet clinical standards, and use the information technology systems the Ministry is developing. However, district health boards will have some discretion over how they administer the vaccines to best meet the needs of their communities. Some primary health care providers, such as GPs, will also be involved. However, we understand that district health boards will make decisions about the extent of their involvement.
4.51
The Ministry asked each district health board to develop plans for how they propose to administer vaccinations in their communities, in line with the design specifications that the Ministry has set. In December 2020, the Ministry asked district health boards to start providing information about their preparedness for vaccine delivery, which they were required to respond to by January 2021.
4.52
Since then, district health boards have been required to provide a series of plans that show how they will progressively administer more vaccinations. The Ministry considers whether plans are adequate, by looking at whether:
- they have considered how to ensure equitable access;
- the required workforce for their vaccination sites has been identified and secured; and
- they can demonstrate how they plan to scale up.
4.53
The Ministry told us that district health boards will also be required to provide separate workforce plans in the future.
4.54
Some of the district health boards’ plans have been more comprehensive than others. We understand that the Ministry is providing support to some district health boards to help them with their planning. This has included seconding someone to work directly with a district health board.
4.55
Before a new vaccination site is used, district health boards must do a “dry run” (without the vaccine) and a “wet run” (with the vaccine). The district health board chief executive or their delegate is required to sign off a checklist confirming that a site is ready. The signed checklist needs to be submitted to the Ministry before it will authorise vaccines to be delivered to the site.
4.56
The short lead time for developing these plans means some district health boards might not have engaged enough with health care providers in their areas to determine the best way to reach specific communities – for example, Māori and Pasifika communities and people with disabilities. If that continues to be the case, there is a risk that equity objectives will not be met in some parts of the country.
Assurance and risk management
The programme is supported by real-time assurance and advice
4.57
Shortly after it was set up, the Governance Group advised the Ministry that more assurance was needed over the immunisation programme. Because of the speed with which the programme needed to move, traditional assurance, such as Independent Quality Assurance reviews, was not considered immediate enough. Instead, in December 2020, the Ministry appointed two external people with relevant seniority and experience to provide real-time assurance and advice to the programme.
4.58
The assurance providers are embedded in the immunisation programme and have ready access to people and information. They attend Governance and Steering Group meetings and other meetings where relevant. They have considered issues at a programme-wide level, but also looked into parts of the immunisation programme in more detail.
4.59
Senior staff from the Ministry and members of the Governance Group told us that they have found the input from the assurance providers helpful. Input has been timely and made directly to the people that need to hear it. The assurance providers track the key findings from their work and report to the Ministry as they identify issues. The minutes of Governance Group meetings we saw included a record of advice being given by the real-time assurance providers. The Ministry provides information to both the Steering Group and Governance Group about the actions it intends to take in response.
4.60
In early April 2021, the real-time assurance providers adapted their approach so that they could focus on areas that needed more attention. These areas were: programme structure and leadership, reporting, public communications, communication with the health and disability sector, the vaccination workforce, and the booking system.
4.61
The real-time assurance providers also recommended that they focus on providing assurance over the extent to which an equity approach has been developed and embedded, and the identification and management of privacy and security risks.
4.62
In other areas, where more progress had been made, the real-time assurance providers recommended that the immunisation programme start to provide its own assurance. These areas included programme design, roles and accountabilities of district health boards, continuous improvement, logistics and finance, and funding. The Ministry told us it is putting an assurance framework in place to support this.
The risk management approach is sound
4.63
The Ministry engaged an experienced risk manager to lead the programme’s risk management approach in mid-February 2021. This was in response to feedback from its assurance advisors that there was not an adequate risk-management approach embedded in the immunisation programme.
4.64
There is now an improved risk management approach in place. Risks have been identified and mapped to relevant workstreams and across the immunisation programme as a whole.
4.65
Mitigation and management strategies are being regularly identified, and progress is reported weekly to the Steering Group and fortnightly to the Governance Group. We saw evidence that the Steering Group makes decisions to address risks as required, for example:
- Additional staff were engaged to assist with managing key person risk, including the addition of a second Programme Director to work closely with delivery leads.
- In response to concerns raised about the clarity and alignment of external messaging, a review was carried out and changes were made to improve communications planning and output.
- In response to risks being escalated about unclear accountabilities, the immunisation programme’s structure was reviewed and the number of Senior Responsible Officers reduced.
4.66
The approach appears to be working. It has identified the main risks to the immunisation programme that we would expect and largely reflects the issues we discuss in this report. Risk management reporting is being actively used by the Steering Group to identify and take action to reduce or resolve risks and issues. In our view, if this approach had been in place earlier, it could have helped resolve some of the issues that the immunisation programme is now facing.
Some risks require more attention
4.67
In our view, the risk management approach that is in place also highlights how much planning and design work is left to do before the immunisation programme will be ready to fully scale up. We consider that there are still risks that the programme should give more attention to:
- Matching demand for vaccine with supply to minimise wastage – the Ministry needs to focus on getting reliable systems to forecast demand as accurately as possible and track inventory in real time. The work under way to make sure the distribution model is fit for purpose and flexible enough to transport doses of the vaccine between sites is critical to minimising waste.
- Securing and training enough vaccinators – at the time we completed our audit, it was still not clear how big the workforce needs to be or where it will be sourced from.
- Meeting equity objectives – although there has been considerable focus on Māori and Pasifika communities and, more recently, people with disabilities, there is limited focus on other groups where there might be equity concerns, such as migrant communities, those with mental health issues, older people, and homeless people. We are concerned that there is little time to properly factor equity considerations into implementation. The risk we see is that district health boards and health care providers could ultimately focus on throughput of vaccinations over sequencing or equity considerations.
- Maintaining overall trust and confidence in the immunisation programme – the Ministry has started to be more transparent with the public about the significant challenges the programme faces and the level of uncertainty that still exists. We strongly encourage this to continue because, in our view, transparency is an important way to build public confidence.
4.68
The Ministry told us that although there could be some changes in timing in delivering aspects of the immunisation programme, it does not think that this will change the overall time frame for completing the programme.
4.69
Current district health boards’ plans anticipate a daily vaccination rate of up to about 18,000 by the end of June 2021. We understand that this reflects both the supply of vaccines and the system capacity in place. For the remainder of 2021, the daily vaccination rate will need to increase significantly for the immunisation programme to be completed by the end of the calendar year.
4.70
The Ministry’s forecasting shows the immunisation programme will need to deliver up to about 76,000 doses each day for a period of seven weeks in September and October. This assumes that vaccines are administered seven days a week.
4.71
Our view at this stage is that we expect the nationwide vaccine roll-out to scale up, but it could take more time than currently planned and there are likely to be some problems. To a degree, this is expected with a programme of this scale. It will be important to have effective processes to identify, escalate, and resolve issues as they arise.
More focus on contingency planning is required
4.72
As well as the risks we describe above, planning is still based on several important assumptions including:
- the vaccine will be delivered to New Zealand in relatively even instalments for the remainder of 2021, and it will all have arrived by the end of 2021;
- enough vaccinators and support staff (who are required to, among other tasks, check people in and to enter details into the Covid-19 Immunisation Register) will be able to be identified and trained to support the scale-up;
- a fit-for-purpose distribution and inventory management system and booking system will be ready in time;
- the immunisation programme will not be disrupted by further community outbreaks of the Covid-19 virus; and
- the vaccines purchased continue to be effective, including against any significant new variants of the Covid-19 virus.
4.73
We saw documents that set out how the sequencing of vaccinations could change in three community transmission scenarios. On 29 March 2021, advice was provided to the programme Steering Group that indicated it was likely that a “ring” vaccination approach would be required in an outbreak scenario – that is, to immediately vaccinate those most likely to be infected by a confirmed case – and that an acceleration of the roll-out plan might be desired.
4.74
The advice also recommended further work to develop contingency plans to enable the immunisation programme to respond in the event of community transmission. We agree, and we consider that this needs to be progressed with urgency. By this stage in the immunisation programme, we would expect contingency planning to be much further advanced.
4.75
We have not been provided with contingency plans that set out how to respond if the risks described earlier in this section become issues, or if other planning assumptions prove to be incorrect. The consequences might simply be that the roll-out will take longer. Nonetheless, we consider it important to have clearly thought through the likelihood and implications of each scenario and how the immunisation programme will respond.
| Recommendation 2 |
|---|
| We recommend that the Ministry of Health complete contingency plans for major risks, for example, vaccine doses do not arrive in New Zealand at the scheduled time or in the expected quantities, adequate workforce is not able to be secured, key systems are not ready on time, or a community outbreak of Covid-19. |
11: Te Tiriti responsibilities involve protecting the rights of Māori and implementing the five Wai 2575 principles of tino rangatiratanga, equity, options, active protection, and partnership in the immunisation programme.
12: Individuals responsible and accountable for the successful delivery of a programme.
13: The Vaccine Ministers comprise the Prime Minister, Minister of Finance, Minister for Covid-19 Response, Minister of Health, Minister of Foreign Affairs, Associate Minister of Health (Māori Health), and Minister for Pacific Peoples.

