Part 6: How were the national reserve supplies distributed?
6.1
Supplying PPE is part of the day-to-day routine of providing health services. It is also a vital part of responding to a health emergency such as Covid-19. Maintaining adequate stock of PPE on hand ensures that critical health services are able to continue to operate safely even if supply chains are disrupted in an emergency.
6.2
The Ministry told us that, before Covid-19, it had no day-to-day role in distributing PPE. In this Part, we discuss the changes that the Ministry made to centralise the supply and distribution of PPE to DHBs and other providers.
Centralised ordering and distribution
6.3
Initially, the Ministry did not know what PPE stock DHBs held or how quickly that stock was being distributed. At the Covid-19 daily briefing on 26 March 2020, the Director-General of Health said that the Ministry would make PPE supply and distribution a national process.
Ordering and allocation
6.4
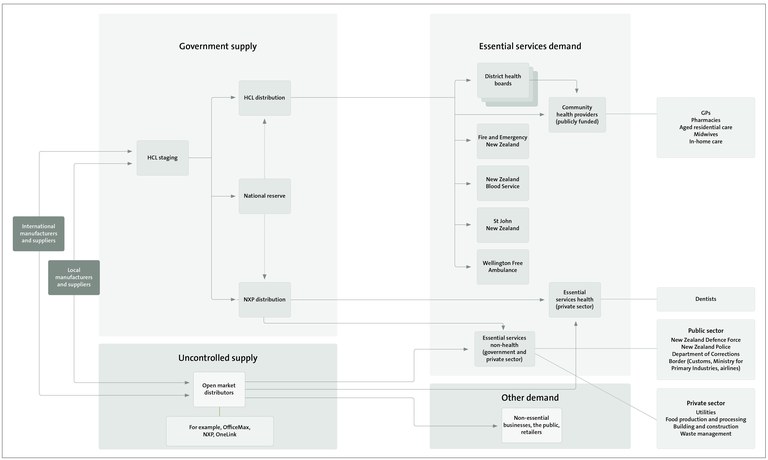
From 1 April, all nationally procured stock was routed through Healthcare Logistics (HCL). HCL and OneLink (a health supply chain company) have more than 20 years’ experience as healthcare distribution providers, mostly working with manufacturing companies. They have supply chain management contracts throughout New Zealand.
6.5
HCL already had a contract with the Ministry to store pandemic pharmaceutical supplies. The Ministry extended this contract to include warehousing and logistics for PPE.
6.6
Under the new system, DHBs, community health providers, and other essential health workers requiring PPE could (with Ministry approval) set up an account with HCL that gives them access to an online portal to request an allocation of PPE. The Ministry reviewed the orders to gain a comprehensive view of national demand, urgency, and stock on hand.
6.7
To manage potentially competing demands for PPE, the Ministry prepared a prioritisation process for deciding how PPE should be allocated. This process assessed PPE requests from DHBs and organisations that are not part of the health and disability sector. The Ministry’s criteria took into account:
- the criticality of the service asking for the PPE;
- how much stock was available and on order, and usage rates (to minimise the risk of supply shortages); and
- urgency of need throughout the country (to balance competing demands).
6.8
From 1 May 2020, the Ministry’s new centralised process for ordering PPE applied to all orders.13 DHBs were told that all orders from domestic suppliers would be redirected to the Ministry under the new national model. Stock was moved to particular warehouses to be made available for distribution through the national model.
6.9
The Ministry made these changes so it could manage stock levels nationally to ensure that PPE was available when and where it was needed.
National stock distribution system
6.10
Before Covid-19, a company called HealthSource provided shared services for supply chain management to the four northern DHBs (Auckland, Waitematā, Counties Manukau, and Northland).14 HealthSource contracted Onelink to manage its stock as a warehouse and logistics provider. OneLink provided internal supply chain and distribution (including supplies for operating theatres and stock management) for the northern DHBs, Waikato DHB, and Southern DHB.
6.11
QSi are contracted to manufacture, store, and distribute national reserve masks to DHBs. However, before Covid-19, there was limited call on QSi’s store of masks. The Ministry contracts other providers to store and distribute other national reserve items.
6.12
During Covid-19, two methods of distribution were implemented for publicly funded health care providers. PPE could be distributed to the DHB or ordered by the DHB on behalf of the provider and delivered to that provider directly. From the second week of April, health care providers could also place orders through HCL using the Onelink portal. The Ministry would review the order and authorise the release of PPE for direct distribution to the provider.
6.13
The Ministry engaged National Express Products (NXP, a sourcing and distribution company) to provide a distribution service (primarily for masks and gloves) to essential workers who are not part of the health and disability sector. Private organisations could register and order PPE supplies through NXP, which were offered at cost plus any distribution costs. This was initially restricted to general purpose and N95 masks.
6.14
In practice, the DHB supply processes did not change, apart from adding new providers and dealing with increasing demand. Distribution from DHBs to community health and disability care providers varied – some DHBs preferred to order on behalf of the provider and have HCL deliver the PPE directly to the provider. Other DHBs preferred to have the stock sent to them to distribute to health care providers.
6.15
On 9 April 2020, the Ministry of Business, Innovation and Employment engaged Mainfreight Limited as the preferred freight provider for international air freight and domestic distribution services. Mainfreight Limited delivered PPE to New Zealand sites, as directed by the Ministry.
6.16
Figure 3 shows the distribution process that developed during the response to Covid-19.
Figure 3
Distribution process for personal protective equipment, developed during the response to Covid-19 (Click on the image to see a larger version of it.)
6.17
On 1 May 2020, the Ministry formally advised DHBs that HCL would distribute PPE to national service organisations such as St John, Wellington Free Ambulance, air ambulance services, Fire and Emergency New Zealand, New Zealand Blood Service, New Zealand Health Group, Manawanui, Access Community Health, and Green Cross Pharmacies. Dentists providing emergency services could access PPE through DHBs.
Getting personal protective equipment to community providers
6.18
The Ministry told us that during March 2020 it released masks from its national reserve to DHBs as demand for masks was increasing. On 31 March 2020, the Ministry released 1.2 million general purpose masks from the national reserve for DHBs to distribute to health and disability providers. The Ministry asked the DHBs to set up processes to distribute PPE to all local publicly funded health and disability providers, including those not directly funded by the DHBs (this included a mix of private businesses, non-governmental organisations, and providers contracted by the Ministry).
6.19
The Ministry said that it would distribute 1.2 million general purpose masks from the Ministry’s national reserve to DHBs and that further masks would be transferred during the next two weeks. On 31 March 2020, the Ministry instructed DHBs that:
We need you to establish a local process today for the distribution of PPE to all publicly funded health and disability providers who deliver health and disability services (Aged Care, Home and Community Support, Disability support services, Community based providers, Midwives etc) This includes providers who may not be directly funded by DHBs, such as MSD and ACC providers.
We need you to communicate this process to providers in your district in the next 24 hours. To ensure providers get the masks they need as fast as possible, you must start using masks from your reserves while we distribute new masks to you. This needs to be done with urgency. We will provide you with recommended volumes of PPE for providers of different sizes tomorrow.
Providers will need to be aware of the current published clinical guidelines which have not changed. DHBs need to reinforce to providers that when they allocate to health care workers, that [health care workers] need to have the requisite training for using masks in order to mitigate any risks of further transfer of the virus. …We recognise this means you will be providing a service to a number of organisations that you would not normally do so. However, we are dealing with a situation that requires us to operate differently.
6.20
The Ministry emailed disability providers and the Needs Assessment Coordination Services (organisations contracted to work with people with disabilities, their families, and carers) advising them that DHBs would contact them to ascertain their PPE needs.
How did the district health boards approach this?
6.21
We looked at how five DHBs approached this. Our observations are high level – we would need to do more work with all DHBs to understand how they managed provider requests and how hospitals prioritised how they used PPE internally and supplied it to the community-based health and disability sector.
6.22
It is clear that the DHBs took different approaches to fulfilling this instruction (for example, providers reported finding it easier to access PPE in some areas than others). Each DHB had its own process for receiving requests from community providers, reviewing and clarifying requests before processing, assessing demand, recording the PPE it released, and releasing PPE.
6.23
Waikato DHB asked community providers to confirm how many staff the provider had who would need PPE, their roles/tasks that would need PPE, and how much PPE would be needed (based on clinical guidance at the time).
6.24
Capital and Coast DHB told us that before the Ministry’s email it had already distributed PPE to primary health organisations on 18 March 2020, and to other community providers from 27 March 2020. Capital and Coast DHB told the Ministry that it would co-ordinate requests for PPE from community providers in the Capital and Coast DHB, Hutt Valley DHB, and Wairarapa DHB areas. The DHB emailed community providers on 2 April 2020 outlining the process for ordering PPE.
6.25
Capital and Coast DHB prepared a request template and set up a central email address to receive requests. Community Based Assessment Centres (CBAC) and primary care requests were to be expedited.
6.26
Capital and Coast DHB treated requests from aged residential care providers differently. A stocktake of aged residential care PPE was to be carried out, and minimum levels of PPE were established with infection control staff. The level of PPE took into account requirements to isolate newly received patients and to isolate suspected Covid-19 patients. The DHB said that, if aged residential care providers had not made enough provision for PPE, it would provide more.
6.27
We also saw templated emails from Southern DHB dated 17 and 27 April that referred the reader to Ministry guidance for community-based workers. The templated message said that there was high demand for PPE and that the DHB had been able to obtain only enough supplies to maintain DHB services.
The DHB told us that it did not receive any of the masks released by the Ministry on 31 March 2020.
6.28
In most instances, Southern DHB informed these providers that the only PPE requirement relevant for them was fastidious hand hygiene. The DHB suggested that providers contact private medical suppliers or NXP. We were told that the DHB sent this response to non-funded health and disability providers and essential workers who are not part of the health and disability sector. However, in April, the DHB provided some PPE to aged residential care, midwives, and disability services.
6.29
Canterbury DHB told us that it did not receive any masks from the Ministry in February or March 2020. On 1 April 2020, it told community providers that PPE was being prioritised to hospital workers, health centres, general practitioners, and rest homes. It also told them that good handwashing and maintaining distance was the best way of avoiding infection.
6.30
However, we also saw evidence that, on 16 April 2020, Canterbury DHB distributed masks to disability, aged, and mental health residential care facilities and to six home-based support service providers. The DHB told us that this was a once-only allocation and that, unless the provider or service was dealing with a suspected or confirmed Covid-19 patient, the DHB would not provide any more PPE.
6.31
Staff from the four northern region DHBs and HealthSource worked together at the Northern Region Health Coordination Centre based at Auckland DHB co-ordinating PPE requests on behalf of Waitematā DHB, Counties Manukau DHB, and Northland DHB. We have viewed an undated letter that informs community providers about a new process for requesting PPE. The letter said that the release of N95 masks would need to be clinically approved.
6.32
We can see from the information provided to the Minister’s rapid PPE stocktake (see paragraph 6.40) that the DHBs provided supplies to aged residential care facilities. However, these supplies were not necessarily in the quantities that were requested. One provider asked for 17,500 masks (10,000 were supplied), 5000 gowns (125 were supplied), and 2000 units of eyewear (25 were supplied).
6.33
DHBs were faced with balancing prioritising supplies and preventing providers from stockpiling PPE in quantities that they were unlikely to need.
6.34
We saw evidence of some inconsistency in DHBs’ approaches to supplying PPE to community health providers. In some instances, DHBs told community health providers that they were not in a position to supply PPE. We acknowledge that DHBs were being asked to do something during a national crisis that had not been planned for and that they had not done before.
What did service providers tell us?
6.35
A nationwide service provider that supports people with disabilities who have individualised care funding from the Ministry told us that it found dealing with multiple DHBs to access PPE frustrating and inefficient.
6.36
The provider told us that the Ministry had agreed to identify what PPE the provider’s staff would need and that it understood that the PPE had been provided to DHBs for distributing. Two DHBs would not provide the PPE requested, and another released 10% of the PPE that the organisation thought had been agreed with the Ministry.
6.37
As a national organisation, the provider considered that it made more sense to deal directly with the Ministry rather than with 20 DHBs.
6.38
In Part 3, we describe how clinical guidance on PPE use by community health and disability support workers changed between March and May. When the Ministry asked DHBs to distribute PPE to community based providers, DHBs were still applying the 31 March guidelines, which took a more restrictive approach to when PPE was needed.
6.39
The New Zealand Spinal Trust told us that, in early April 2020, it asked all DHBs how PPE could be obtained for people with spinal cord injury living in the community to provide to their carers. Two DHBs said that they had already supplied some PPE to spinal cord injured people who had contacted them directly. All but two of the other DHBs made it clear they would issue PPE only in accordance with the Ministry’s clinical guidance (that is, only to confirmed or suspected Covid-19 patients).
What did the Ministry of Health’s rapid personal protective equipment stocktake find?
6.40
On 23 April 2020, the Minister of Health asked the Ministry to conduct a rapid stocktake of what PPE DHBs had distributed to community health and disability providers.15 DHBs were asked to report:
- what PPE they had distributed to community providers during the previous two weeks (the DHBs were not asked for information about what providers had requested, only what they had distributed);
- how PPE was ordered and distributed, and the time frame for this; and
- the complaints process, complaints received, and how the DHB addressed them.
6.41
This review provided a snapshot of how the system was working towards the end of April, after revised ordering and distribution systems had been set up. Because the review focused only on this time period, it is unlikely to have captured a full picture of the experiences of providers.
6.42
The information provided by DHBs as part of the rapid PPE stocktake indicates that the DHBs’ approach to providing PPE to community providers still varied considerably in late April. The Ministry acknowledged that DHBs had worked to set up distribution for providers that they did not have a previous relationship with and that, although there had been “teething problems”, these were mostly resolved.
6.43
The Ministry told us that it felt that some DHBs took some time to recognise the scope of the disability sector (that is, disability residential care and people with individualised care packages). This was the first time significant contact DHBs had with these Ministry-funded disability support providers and disabled people with individualised funding.
Our observations
6.44
Although the devolved system of managing PPE stock and distributing it to the health and disability sector may have worked well under normal circumstances, it was not able to manage the increased flow of stock needed during the Covid-19 response.
6.45
The Ministry needed to act quickly to set up a centralised approach to managing national reserve stock levels, ordering, freight, and distribution. With the benefit of hindsight, having these systems and processes in place at the outset would have enabled the Ministry to respond faster and make better-informed decisions about supply and demand challenges.
6.46
The Ministry responded appropriately by setting up a new centralised system for prioritising, allocating, and distributing PPE stock. It could improve some weaknesses in that system, including that it remains difficult to reconcile stock volumes and stock distribution.
| Recommendation 9 |
|---|
| We recommend that the Ministry of Health, in collaboration with district health boards, prepare more detailed operational plans and processes that describe how the national reserve system should operate (including distribution mechanisms) and test these as part of future national health emergency exercises. |
6.47
In late March 2020, the Ministry asked the DHBs to set up processes to distribute PPE to all local publicly funded health and disability providers, including those not directly funded by the DHBs (this included a mix of private businesses, non-governmental organisations, and providers contracted by the Ministry).
6.48
The DHBs we looked at did this. We saw that there were delays in early April in providing PPE to community-based providers, but by late April the DHBs we looked at had distributed PPE to community providers. This is consistent with the findings of the rapid stocktake of PPE requested by the Minister.
6.49
We heard concerns from community health and disability providers who sought to access PPE through DHBs. We heard about different approaches to allocation, particularly in early April and particularly for health providers that the DHB had no pre-existing relationship with. We saw correspondence from DHBs to one nationwide community disability support service indicating that it would not provide PPE to them. In early April, health and disability workers in different DHB areas were getting different responses about what PPE they could expect to receive.
6.50
We consider it important to note that DHBs were being asked to do something during a national crisis that had not been planned for and that they had not done before. It is not surprising that there were challenges for DHBs in setting up these processes in a short time.
6.51
We would need to do further work to identify how different DHBs treated requests from community-based health providers and form a more comprehensive view on the extent of this. We will consider whether to do further work to better understand this.
13: The Ministry’s demand model informed the quantities of PPE to be purchased. Procurement leads at Auckland, Waikato, Capital and Coast, Canterbury, and Southern DHBs submitted a request to a designated Ministry finance team member, who raised and approved an electronic purchase order with the supplier. Once the procurement lead confirmed receipt of goods/services, they advised the Ministry’s finance team that payment could be made.
14: In addition to providing a shared service for procurement and supply chain, HealthSource also provided a shared service to the four Northern DHBs for finance, payroll, and eligibility assessments.
15: Hon Dr David Clark (23 April 2020), Rapid stocktake of PPE distribution, available at www.beehive.govt.nz.