Part 1: Introduction
1.1
In this Part, we discuss:
- the purpose of our audit;
- the context for regional services planning;
- the intended effects of regional services planning;
- how regional planning works in the health sector; and
- how we carried out our audit.
The purpose of our audit
1.2
In our annual plan for 2012/13, we proposed to audit the leadership that the Ministry of Health (the Ministry) provides to district health boards (DHBs) in co-ordinating asset management throughout the health and disability sector and integrating it with service delivery, including how this affects how DHBs manage assets.
1.3
In scoping our work, we saw that models of service delivery were being reconsidered to help ensure the future sustainability of the health and disability system. DHBs were being encouraged to collaborate regionally and sub-regionally where it made sense to do so (see Figure 1). This policy would inform DHBs' long-term investing in major assets, such as hospitals.
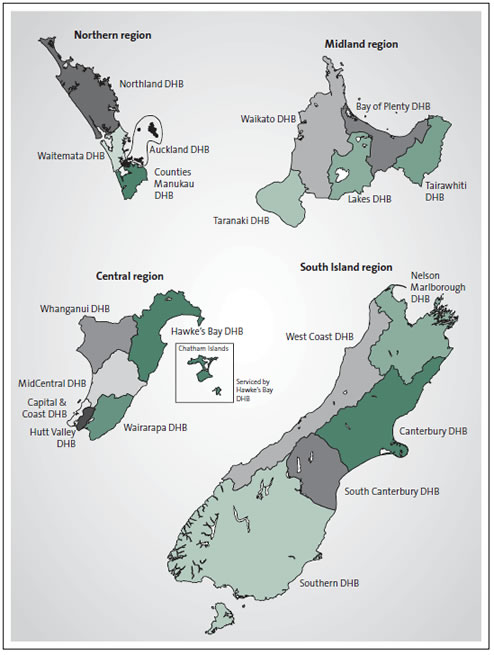
Figure 1
Map of the four health sector regions and their district health boards
District health boards are grouped into four regions – Northern, Midland, Central, and the South Island. The regions’ populations range from about 850,000 to 1.7 million people.
1.4
We learned that regional services plans would be strategic documents setting out changes in service delivery, and would increasingly influence decisions about capital investment. Therefore, we decided to look at the leadership the Ministry was giving to DHBs on regional services planning and what that planning was intended to achieve.
1.5
We maintained a focus on service delivery, capital investment, and the availability of good quality data that would support decision-making in those aspects.
The context for regional services planning
1.6
The Appendix shows the present structure of New Zealand's health and disability sector, the major public entities in the sector, and the relationship between those public entities.
1.7
In 2009, a Ministerial Review Group (the Review Group) reported to the Minister of Health (the Minister) through a report called Meeting the Challenge: Enhancing Sustainability and the Patient and Consumer Experience within the Current Legislative Framework for Health and Disability Services in New Zealand.1
1.8
The Minister asked the Review Group to identify what would:
- improve performance and quality in health and disability services;
- improve the health system's capacity to deliver services; and
- increase spending to support frontline care by reducing back-office costs.
1.9
The Review Group reported that:
Unless we change the way services are provided, it will become increasingly difficult to meet public expectations for improved service within a sustainable funding growth path.
1.10
Simply put, as a country, we would not be able to afford New Zealanders' future health needs if nothing changed. The Treasury's 2013 report on long-term government finances showed that health care spending is projected to grow from 6.8% of Gross Domestic Product in 2010 to 10.8% in 2060.2
1.11
The Review Group's report highlighted many opportunities to:
- reduce costs by reducing fragmentation and duplication of services (which had arisen because of having 20 autonomous DHBs);
- reduce variations in the quality of care and access to elective (planned) surgery between DHBs and within regions;
- reduce the risk of some "vulnerable services" collapsing;3 and
- prevent local interests of individual DHBs taking inappropriate priority over regional or national planning.
1.12
The Review Group proposed changes to:
- encourage changes in culture and ways of working in DHBs, including better integrating primary care and hospital-based care; and
- introduce national support structures to help reduce waste, improve safety and quality, and enhance clinical and financial viability.
1.13
In response, the New Zealand Public Health and Disability Act 2000 was amended, and new planning regulations came into force on 1 June 2011. Among the Review Group's recommendations that were put in place were:
- setting up the National Health Board (NHB), supported by specialist advisory committees to deal with matters such as workforce, information services, and capital investment;
- requiring DHBs to plan sub-regionally or regionally;
- DHBs putting in place the governance and support arrangements to deliver those plans; and
- the Minister acquiring the power to direct DHBs on matters to do with delivering regional services.
1.14
The Review Group found a strong consensus in the health sector about making the DHB model work better. Regional services planning was introduced into a complex system as an alternative to structural change for the 20 DHBs. Funding and governance arrangements were kept much as before, which offered stability to the sector. The Review Group saw advantages, in that DHBs could get regional planning under way immediately, without losing time and effort that might otherwise have gone into restructuring.
1.15
However, the Review Group was not certain that the changes it recommended would take the sector "far and fast enough". Based on a Review Group recommendation, Cabinet agreed to a review of the DHB model within three years. This would assess:
… whether more fundamental reform will be needed to create strong enough incentives for efficiency and to enable the sector to lift its performance within a more sustainable growth track.
Intended effects of regional services planning
1.16
Regional services planning requires DHBs to work together, and with other health providers, in a more integrated way. The regional services plans outline how DHBs will plan, fund, and deliver services regionally to:
- reduce service vulnerability;
- reduce cost; and
- improve quality of care.
1.17
The Ministry's guidance is that it is up to DHBs to plan services, but, in doing so, they must consider what services are appropriate and financially sustainable for the size of the region's population.
How regional planning works in the health sector
1.18
The NHB is responsible for:
- funding and monitoring DHBs and overseeing their planning (such as annual funding and planning rounds, including regional services planning);
- bringing together various aspects of the health delivery system (information technology, facilities, planning) so that they work together in a way that will meet health service needs;
- providing guidance on which services should be planned, funded, and provided nationally, regionally, and locally, and how that should change over time; and
- ensuring that regional services planning is in line with decisions about capital investment and workforce capacity.
1.19
The NHB is supported by a dedicated business unit within the Ministry. In this report, we refer to the Ministry unless we specifically mean the NHB.
1.20
Specialist committees support the NHB. In this report, we refer to:
- the Capital Investment Committee (CIC), for capital investment decision-making;
- the National Health Information Technology Board (NHITB), for information technology investment; and
- Health Workforce New Zealand (HWNZ), for health workforce planning.
1.21
We also refer to Health Benefits Limited (HBL). This is a Crown company set up to work with the health system to achieve $700 million of savings in its first five years by reducing administration and support costs.
National Health Board regional services planning guidance
1.22
The Review Group's report in 2009 was followed by the Health Sector Framework 2010.4 This contains an outline of the intended legislative and regulatory changes following on from the Review Group's report. The framework envisages that the Ministry will prepare resources (such as planning templates and guidelines) to help DHBs reduce the costs of planning, and to better integrate health planning at different levels of the health sector.
1.23
The Ministry has taken an evolutionary approach to introducing regional services planning since the New Zealand Public Health and Disability (Planning) Regulations 2011 came into effect on 1 June 2011. The Ministry publishes an annual guidance document to guide DHBs on the minimum content of regional services plans, based on the regulations. The guidance is detailed, and regions are able to include more information if they wish.
1.24
The Ministry did not issue regional services planning guidance in 2011/12 as part of the overall planning pack for DHBs.5 Instead, guidance was given:
- in a letter;
- by way of conversations with DHBs; and
- through aspects of the operational policy framework document (a set of business rules and policy guidelines by which all DHBs must work).
1.25
The first regional services plans were prepared in 2011/12. That year was seen as a "transitional year", given that the regulations requiring regional services plans came into effect only a few weeks before the start of 2011/12. The Review Group's report and subsequent Cabinet papers saw a focus on planning and funding vulnerable services as a priority for the content of the first-year regional services plans, and this was reflected in the Ministry's requirements.
1.26
The Ministry identified 2012/13 as a "step increase" year, and 2013/14 as a "comprehensive and detailed" year for regional services planning.
1.27
The Ministry chose to have this phased approach, because not all DHBs and regions were ready to work consistently at a regional level. Some DHBs had worked well at a regional level before the introduction of regional services plans. However, the Review Group had found that the improvements arising from the natural evolution of regional collaboration were slow and uneven, and considered that regional services plans would be the way to lock in and accelerate progress.
1.28
The Ministry monitors aspects of performance against the regional services plans four times a year. It selects topics to discuss further and gives comments in writing (a letter and a dashboard report) and has telephone discussions or face-to-face meetings with lead regional DHB chief executives. The Ministry can take a more challenging approach if it considers progress to be slow.
How we carried out our audit
1.29
We carried out our audit by looking at regional services planning in the South Island and Northern regions. We chose these two regions because:
- they have different characteristics and face different challenges, so looking at these two regions would give us a clear sense of whether the system for planning was flexible enough to encompass these differences; and
- the Ministry told us that most of the medium-term health capital investment in buildings would take place in those regions.
1.30
We collected our evidence in three ways:
- We interviewed 90 people from DHBs, regional organisations, the CIC, the Ministry, and the DHB shared-services organisation.
- We reviewed more than 550 documents and analysed financial information that the Ministry provided to us.
- We audited patient records in four DHBs. We did this to test the quality of the raw data available from DHBs' information systems. Looking at the way data was recorded, collected, and collated enabled us to see how easy it was to get good quality information to inform planning. We chose a new measure (see paragraphs 5.17-5.22) because we were interested in seeing what data was like without significant, and targeted, additional investment of cost and time.
1.31
It would not have been cost-effective to audit every workstream in the regional services plans. Instead, we looked broadly at regional services planning and then at the workstreams relating to capital investment decisions for buildings and cancer treatment.
1.32
Using capital effectively and efficiently is important, especially when large amounts of money are involved. Our investigation into capital focused mainly on investment in buildings. This is because:
- investment in buildings has long-term ramifications for health services;
- capital funding is constrained because the Government aims to return to budget surplus in 2014/15 and beyond (so it is more important than ever to prioritise investment); and
- borrowing to fund capital projects already contributes to some DHBs' deficits.
1.33
We chose cancer treatment because it is a service of great importance to New Zealanders. Cancer is the leading cause of early death in New Zealand. In 2009, more than 20,800 people were diagnosed with cancer in New Zealand and 8437 people died of the disease. Shorter waits for cancer treatment has been a health target for the period that regional services planning has been in place. Regional cancer-services networks were set up in 2006 and 2007. They lead service improvement and planning, support the achievement of health targets and policy priorities, and link to national and regional governance structures. We discuss these networks more fully in Part 4.
What we expected to find
1.34
This is the third year of regional services planning, with two years of plans delivered and the third year's plans agreed. Given the Ministry's intention to ramp up efforts in years two and three (see paragraph 1.26), we expected to find:
- evidence that the plans were achieving their intended effects, as defined in the guidance supplied by the Ministry (these effects include improvements in resilience and quality of service, and reduced costs, as well as changes in behaviour in DHBs);
- that the Ministry was able to show how effective regional services plans had been in contributing to lifting performance in the health and disability sector;
- that regional services plans are used to help make capital investment decisions for buildings; and
- that relevant and good quality information is used when planning regional services.
1.35
During this audit, we looked hard to find out whether regional service planning was leading to changes, or something else. This meant that we looked for evidence, causes, and effect of change.
What we did not audit
1.36
Our audit focused on administrative planning. We did not audit clinical decision-making or clinical safety. Where we discuss improvements in quality of care, it is about improvements as described by DHBs. We did not test these with patients or service users.
Structure of this report
1.37
In Part 2, we discuss our findings on whether regional services planning is increasing collaborative working between the organisations, networks, and workstreams that make up the health delivery system.
1.38
In Part 3, we discuss our findings on whether regional services plans guide capital investment decisions in the health sector.
1.39
In Part 4, we look at what introducing regional services planning has done to regional cancer-services networks – a long-established workstream with its own funding and lines of accountability.
1.40
In Part 5, we discuss our findings about the availability and reliability of good quality data and information used in regional services planning.
1.41
In Part 6, we look at how the Ministry has led and guided the process of regional services planning.
1.42
In Part 7, we discuss our findings on whether the Ministry knows if regional services planning is delivering the intended effects successfully.
1: The report is available at the Ministry of Health's website, www.moh.govt.nz.
2: The Treasury (2013), Affording Our Future: Statement on New Zealand's Long-term Fiscal Position, available at the Treasury's website, www.treasury.govt.nz.
3: Usually, services are vulnerable because of not having enough specialist staff. However, services can be vulnerable because of circumstances, such as many staff retiring over a short time, being in an isolated area, and overall skill shortages.
4: The Health Sector Framework is available at www.nationalhealthboard.govt.nz.
5: The DHBs' financial year runs from 1 July to 30 June.
page top
