Part 2: Deciding whether an after-hours service is required
2.1
In this Part, we discuss how patients and/or their caregivers:
- decide how urgently they need advice and/or treatment for an injury or medical condition; and
- know where to go for that advice or treatment.
2.2
A person with an injury or medical condition needs to consider whether their need for health care is urgent or can wait. When a person underestimates their health need and waits too long before seeking advice and treatment, their injury or medical condition may worsen. The consequences can include death, longer recovery time, or greater financial costs to the person and the health sector. A DHB can also incur higher costs when a person overestimates their health need and unnecessarily seeks hospital treatment.
Summary of our findings
2.3
People may decide by themselves how urgently they need treatment and/or advice or they may decide in conjunction with a GP or nurse. People may seek advice on how urgently they need treatment or further advice by phoning a telephone advice service and/or by visiting an after-hours service. Telephone advice services may also provide information on what after-hours services are available in a given area at a given time. The after-hours service arrangements in some areas are complicated.
Deciding on the urgency for treatment or advice
Deciding on the urgency of the need for treatment and/or advice may be done directly by people themselves or in conjunction with a GP or nurse.
2.4
The first matter that a person has to consider before travelling to an after-hours service is whether the injury or medical condition can wait or requires more urgent care. They have to decide what level of care or advice they need – telephone advice, an emergency response, a GP as soon as possible, or a GP when the GP is next available. They then have to find out where to go for this level of care or advice.
2.5
Most after-hours services are provided by GPs or nurses. The 2009/10 Service Coverage Schedule (page 15) states that: "First-line assessment and treatment of problems" is "normally nurse/doctor GP services". Generally in this report, we refer to the health professionals and health practitioners who provide after-hours services as GPs or nurses.
2.6
The 2009/10 Service Coverage Schedule requires that:
The decision about urgency of need for medical assistance will be made by the health professional based on their clinical judgment and the individual seeking care.8
2.7
This requirement assumes that, when the decision about urgency is made, a GP or nurse is already involved. The most common way to do this is to use a telephone advice service. The alternative is that a person travels to a GP or nurse.
2.8
The toll-free national Healthline telephone service is a way for people to get advice about whether and how urgently they need treatment for an injury or medical condition. We have not audited the performance of the Healthline service because it is not provided by a public entity.
2.9
In some areas, people may also be provided with telephone advice by phoning their GP after hours. In these areas, GPs have entered into private arrangements with a provider of telephone advice services. We have also not audited the performance of these services.
Obtaining information on what after-hours services are available
The after-hours service arrangements in some areas are complicated. People may obtain information on these arrangements from telephone advice services, DHBs, or providers of after-hours services.
2.10
The arrangements for after-hours services in each DHB vary. The number of services that are available to a person often depends on:
- where in the district a person lives;
- whether it is a weekday or weekend;
- what time it is; and
- which GP or general practice is on the roster to provide after-hours services at the time.
2.11
The arrangements in some localities can be very complicated because of this variation. Figure 1 shows an example of the complexity of after-hours services in one area, with multiple providers and opening hours.
Figure 1
Example of the variety of opening hours for different after-hours services
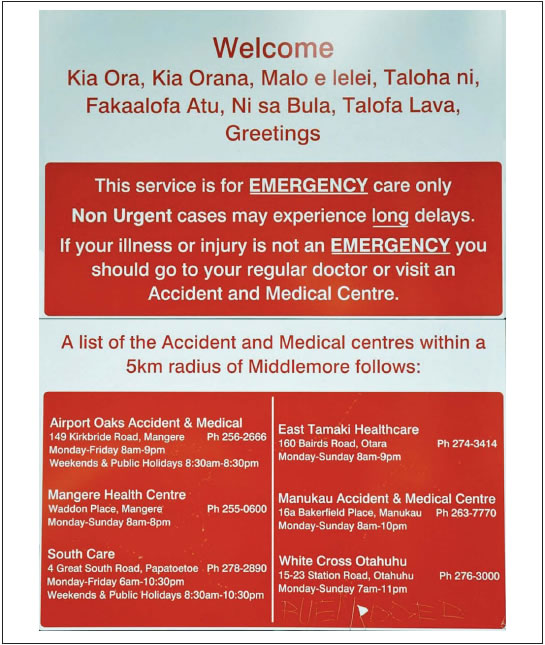
Note: This figure should not be relied on to provide accurate information about after-hours services currently available.
Multiple sources of information on after-hours service arrangements
2.12
People may obtain information on after-hours service arrangements from telephone advice services, DHB-provided information, or providers of after-hours services.
2.13
Healthline is expected to provide information on what services are available in a given area if urgent treatment or further advice is needed after hours. In the 12 months to 31 March 2010, Healthline received more than 18,000 calls (about 5% of its total calls, but not limited to calls about after-hours services) asking for information about health care providers, including their location.
2.14
Other telephone advice services may also provide information on what services are available.
2.15
For some people, access to a telephone may be limited for cost or other reasons. For example, the West Coast DHB's Primary Care After-hours Strategic Plan (2008) notes that poor mobile telephone coverage is managed in Westland by "nurses leav[ing] messages on clinic doors with contact details where possible".
2.16
Most of the DHBs stated in their after-hours plans that they had in place or planned communications to advise patients about availability of after-hours services and how to access them. In several after-hours plans, the main focus of these communications was to promote the use of Healthline or other "nurse telephone services".
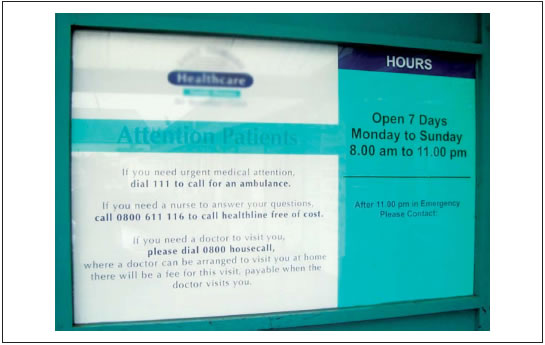
2.17
Where people travel to a service in person, without knowing whether it is available after hours, they may find the service is not available. Where the service is not available, information may be provided at the service about where else the person can go, or who they can contact, for assistance. Figure 2 provides an example of this sort of information.
Figure 2
An after-hours information sign
8: Ministry of Health, 2009/10 Service Coverage Schedule, page 15.
page top